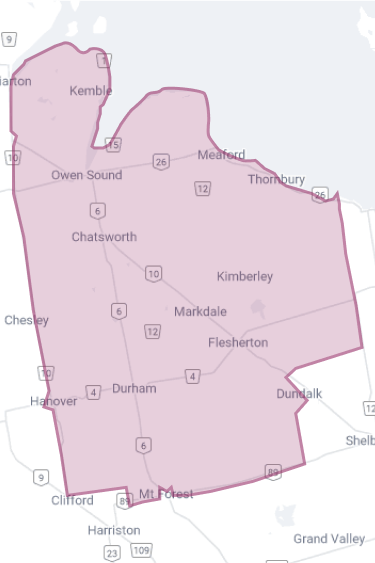
Opioid poisonings decline in Grey County in 2025
Over the past 12 months, opioid related deaths in Grey County have been reduced by 72%, from 18 in 2024 to five in 2025. While year-end provincial statistics for 2025 are not yet available, based on the first three quarters of provincial data, Grey County appears to be showing a reduction in opioid-related deaths and overdoses outpacing provincial declines. Year-end data from Grey County shows 72 suspected opioid overdoses were reported last year compared to 184 in 2024, a reduction of 61%.
Wrap around support and collaboration in local programming are playing an active role in responding to the opioid crisis. Agencies across the region are collaborating and have created a coordinated system of support that responds to the individual needs of those struggling with mental health and addiction.
Supportive Outreach Services (SOS) support community members that are unhoused or precariously housed and suffer from mental health and addictions. These members of the community frequently encounter barriers to accessing services in traditional ways. SOS provides healthcare, counselling, basic needs, and social navigation. They also provide harm reduction supplies and education, and drug checking.
The SOS mobile outreach team includes mental health counsellors from CMHA Grey Bruce, a nurse practitioner from Brightshores Health System, Peer Support Workers who bring lived experience and Indigenous cultural knowledge, community paramedics from Grey County, a social navigator from the United Way of Bruce Grey, as well as a physician who provides consultation in primary care and addictions medicine. Grey Bruce Public Health provides the team with guidance on best practices and overall project direction. The team is further supported by key partners to ensure clients receive comprehensive, wraparound support. Behind the frontline team are more than two dozen partner agencies working together as part of a unified system. Some partners provide direct on the ground support to SOS, while others contribute through referrals that connect clients to municipal, nonprofit, emergency services, healthcare, and social service programs.
"There is no one-size-fits-all approach to solving the overdose crisis, and no community can solve it alone. By investing in community-driven, culturally relevant, and evidence-based initiatives, we are making sure people have access to the care and support they need, close to home."
This unique, collaborative approach to support has been recognised by Western University who shared findings in 2025 from their evidence based, qualitative study that showed that SOS saved lives, that its success was rooted in community and collaboration, and ‘has profound, measurable impacts’ across community.
“The SOS program and other support services in Grey County provide a wraparound approach to providing care. SOS may be the first point of contact providing basic needs and immediate care. As trust is built, clients can be referred to other services for further mental health or medical treatment, or social supports like housing and life skills development,” said Grey County Paramedic Chief Kevin McNab.
While program partners are optimistic about the results in 2025, they also know the issue isn’t solved and more work is ahead. In 2025 the SOS program expanded from three days to provide supports across seven days a week, funded by Ontario Health and Health Canada.
“The 2025 numbers are positive, but they aren’t zero. We know we have more work to do,” says Chief McNab. “Substances in drug supplies are always changing, and we need to stay ready to react and respond. Not as individual services, but as a system of care.”
“A key contributor to Grey County’s progress is the SOS team’s ability to build trust with community members and connect them to treatments and supports that save lives. As relationships grow, the team can introduce options like Sublocade — a long-acting buprenorphine injection that reduces cravings and eases withdrawal symptoms, helping people stay stabilized and less reliant on the toxic, unregulated drug supply,” explains Heather Prescott, Nurse Practitioner with Brightshores Health Systems.
In Grey County, more than 40 community members are receiving Sublocade as part of their treatment goals. This medication provides steady, reliable protection that lowers the risk of opioid poisoning and death. The SOS mobile team can administer it directly in the community for those who cannot access traditional healthcare. Alongside treatment, the team also provides harm reduction supports such as naloxone distribution and education, ensuring individuals, families, and peer networks have the tools to recognize and respond to overdoses. Together, these approaches create safer pathways toward recovery and reduce the likelihood of fatal outcomes.
Grey County Warden Andrea Matrosovs agrees that community interventions are working and encourages partners from around the County to continue communicating and collaborating.
“Taking a collaborative, multi-agency approach to the opioid epidemic is working in Grey County and it’s saving lives,” said Warden Matrosovs. “Local non-profit organizations, hospitals, public health and municipalities have a shared focus on improving the outcomes of those struggling with mental health and addiction in the County. We’re all united and we’re all investing in innovative programs, services and technology that are making a difference.”
-30-
For media inquiries contact Katrina Peredun, communications officer, at communications [at] grey.ca (communications[at]grey[dot]ca) or 519-370-7064.